
Our bodies are pharmaceutical factories. From the hormones that regulate our blood sugar to the neurotransmitters that act as the body’s natural painkillers, these endogenous — produced within the body — chemicals ensure our functionality and survival.
But did you know that our bodies also naturally produce psychedelics?
In the 1950s, researchers found chemical signatures of N,N-dimethyltryptamine (DMT) in mammalian bodies, including in humans.
“When they first identified it, they thought, ‘Okay, maybe this will correlate with schizophrenia diagnoses in some way. If you’ve got really high levels of psychedelics that your body is making, maybe that’s conferring hallucinations and delusions,’” explained Cassandra Hatzipantelis, a postdoctoral fellow at the UC Davis Institute for Psychedelics and Neurotherapeutics (IPN). “But they found no correlation between schizophrenia patients and endogenous psychedelic levels and it was all thrown out.”
Nearly 70 years later, psychedelic compounds are experiencing a medicinal renaissance thanks to their therapeutic properties and ability to promote neuroplasticity.
As IPN Director David Olson — also a professor of chemistry, and biochemistry and molecular medicine — describes it, the brain’s neurons are like a dense tree canopy. In healthy brains, the leaves — the synapses — overlap with one another, but in the brains of those with depression, post-traumatic stress disorder and substance use disorder, among other neuropsychiatric and neurodegenerative conditions, the connections between the neurons are withered.
It’s like a tree in winter: the leaves have fallen from the limbs, but the barren branches are still there.

“Ketamine, LSD, psilocybin, DMT — all these drugs regrow complex neurons within hours, and those benefits last for months,” Hatzipantelis said.
The effects are like an early spring, an acceleration of growth.
IPN researchers are harnessing the chemical structures of psychedelics to design neurotherapeutics that strictly confer these beneficial neuronal effects, divorcing them from hallucinations and any other negative side effects.
As part of that research, Hatzipantelis is navigating the world of endogenous psychedelics while her colleague Yara Khatib, a graduate student in the Olson Lab, is testing a massive library of psychedelic compounds and IPN-developed, non-hallucinogenic analogs. The hope is to accelerate the research pipeline and produce drugs that could readily treat conditions characterized by neuronal damage.
“We have this interdisciplinary setting, where we have biologists, pharmacologists and chemists all working together with one collective objective, and that objective is to understand, neurobiologically, what’s going wrong in various brain conditions and how can we treat that,” Khatib said.
A mystery inside
When it comes to endogenous psychedelics, the list of unknowns is much larger than the list of knowns. Scientists know our bodies make them, but they don’t know how, why or in what scenarios their synthesis is relevant.

“The critical thing here is that the body wouldn’t just make them for no reason,” Khatib said. “They have to be doing something there. There’s a reason they’re being produced. Our bodies are efficient and the fact that everybody has them and at different levels — there has to be something going on, and that’s what we’re trying to figure out.”
Hypotheses abound about the functionality of endogenous psychedelics. The IPN is exploring various possibilities, but one thing is clear, our understanding of neurochemistry is evolving every day. Once staple ideas are now being challenged.
“Dopamine and serotonin are your classic examples of those happy neurotransmitters, but we know that it’s a lot more complex and nuanced than that,” Hatzipantelis said. “We hypothesize that those things that are increasing dopamine or increasing serotonin might actually also be at the same time increasing endogenous psychedelics.”
“They’re incredibly similar structurally to serotonin and we’ve found that they can be stored in the brain like serotonin,” Hatzipantelis added. “It’s possible that whenever our body releases this burst of serotonin, it also releases a microdose of endogenous psychedelics and that’s what’s actually giving the happy feelings, or antidepressant effects.”
It’s possible, according to Hatzipantelis, that those with neuropsychiatric disorders are unable to produce the necessary levels of endogenous psychedelics. She hypothesizes that a neurotherapeutic could act as a kickstarting agent, affecting the body’s natural systems and encouraging natural production. Like many things in the psychedelic realm, the molecular mechanics are still unknown, but IPN is on the case.
“It’s purely hypothetical right now, but we’re trying to answer those questions,” Hatzipantelis said.
A psychedelic library and the development pipeline
In order to accelerate the drug discovery pipeline, Khatib is working on a sprawling project to catalog a comprehensive list of psychedelics and their associated effects on neuronal structure. The goal is to create a method to screen these drugs and classify them based on their effectiveness.
Doing this requires high-throughput screening methods that can screen giant compound libraries. That’s where Khatib comes in.
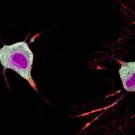
“A big part of what I do is creating these analytical pipelines capable of analyzing thousands of different images from a microscope at once and within like an hour or two, they shoot out the data and tell me, ‘Okay this drug instills this much change versus this other drug,’” Khatib said. “We’re trying to create an automated system that does this.”
Once these effects are determined at the foundational level, the research can be passed to other researchers at IPN, who can use the structural information as a basis for neurotherapeutic design.
For Hatzipantelis and Khatib, the opportunity to be a part of this revolutionary new wave of medicine, and the interdisciplinary nature of the work, is what drew them to IPN.
“I want to make a real difference in my lifetime,” said Hatzipantelis, who traveled across the globe from Australia to work at IPN. “I want to be at a place where I can make new molecules and potentially help patients directly.”
“I never would have imagined myself growing as a scientist in the way that I have in these last three years,” Khatib said. “I think part of that is the collaborative environment that we have at UC Davis as a whole. Everyone has the same objective: to produce knowledge that’s accessible to the world and not to gatekeep that knowledge.”
“We don’t have to rely on waiting for someone on the other side of the world who has that expertise,” Hatzipantelis added. “We’ve got expertise in house, and we can all work together more cohesively, more strategically and more effectively and efficiently.”
YOU MAY ALSO LIKE THESE STORIES
UC Davis Develops Tool to Track Psychedelic Effects on Neurons in Minutes
UC Davis researchers have developed a rapid, noninvasive tool to track the neurons and biomolecules activated in the brain by psychedelic drugs. The protein-based tool, which is called Ca2+-activated Split-TurboID, or CaST, is described in research published in Nature Methods.

Catalyzing Change
Design2Data, or D2D, provides undergraduate students with early laboratory experiences learning about enzymes and related protein structures with findings that contribute to a national network of data. The project is an extension of chemistry professor Justin Siegel’s lab at the UC Davis Genome Center.
